Juniper Publishers - Septic Lyme Arthritis after Recent Anterior Cruciate Ligament Reconstruction
Orthopedics and Rheumatology Open Access Journal
Abstract
It is estimated that in the United States, there are approximately 100,000 primary anterior cruciate ligament (ACL) reconstructions performed yearly. Reports of septic arthritis after ACL reconstruction are rare, ranging from 0.14% to 0.48% in the literature. 1-5 There are no other reports in the current literature documenting the treatment of Lyme arthritis after ACL reconstruction. A 19-year-old male sustained a non-contact injury to his left knee while playing basketball. The patient underwent 6 weeks of rehabilitation and subsequent ACL reconstruction with Achilles tendon allograft. The patient developed Lyme arthritis of the knee three months after ACL reconstruction. The patient underwent urgent irrigation and debridement with retention of graft. At final five-year follow-up the patient had returned to full activity, without complaints. We report on a patient who underwent successful treatment for Lyme arthritis after ACL reconstruction. Even though B. burgdorferi does not produce proteases to digest collagen and other proteins of articular cartilage, joint damage can occur due to the host inflammatory reponse.8 Therefore, in the setting of recent ACL reconstruction without the ability to rapidly distinguish between Lyme arthritis and bacterial septic arthritis, the decision should be to urgently irrigate and debride the joint.
Abbreviations: ACL: Anterior Cruciate Ligament; MRI: Magnetic Resonance Imaging; PCR: Polymerase Chain Reaction; EIA: Enzyme Immunoassay; IKDC: International Knee Documentation Committee
Introduction
It is estimated that in the United States, there are approximately 100,000 primary anterior cruciate ligament (ACL) reconstructions performed yearly. Despite a success rate of 92-98%, ACL reconstruction is not without potential complications, including post-operative infection [1]. Reports of septic arthritis after ACL reconstruction are rare in the literature; with infection rates ranging from 0.14% to 0.48% in the literature. [1-5]. The consequences of septic arthritis can be disastrous leading to arthrofibrosis, chondral damage, arthrosis, and chronic osteomyelitis [1].
The goals of managing septic arthritis after ACL reconstruction are to protect the articular cartilage and the graft [2]. Early diagnosis and treatment is critical to optimizing outcomes. Even with early intervention and graft retention patients can require multiple surgical procedures, with risk of arthrofibrosis, recurrent infection, and poor long-term functional outcomes [5-7]. We present the case of a patient who developed Lyme arthritis of the knee three months after ACL reconstruction with an Achilles tendon allograft. The patient’s clinical presentation was atypical of septic arthritis, aside from a large effusion. Caused by the tick-borne spirochete, Borrelia burgodorferi, there are no other reports in the current literature documenting the treatment of Lyme arthritis after ACL reconstruction.
Case Report
A 19-year-old male sustained a non-contact injury to his left knee while playing basketball. He had immediate pain and swelling, as well as instability with activity. Magnetic Resonance Imaging (MRI) of the left knee was obtained and showed a complete left ACL rupture with associated medial and lateral meniscal tears. The patient underwent 6 weeks of rehabilitation and subsequent ACL reconstruction with Achilles tendon allograft. Intra-operatively the patient was given 1 gram of Ancef within 1 hour of incision, and underwent arthroscopic ACL reconstruction with bio-interference screw fixation in both tibial and femoral tunnels. The concomitant medial and lateral meniscal tears were amenable to repair using Smith & Nephew (London, UK) Fast-fix meniscal repair system. In the immediate post-operative period the patient’s incisions healed without incident and he was started in an early-motion rehabilitation protocol.
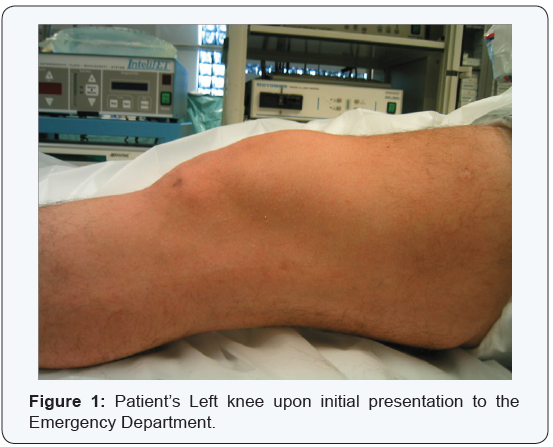
Three months after surgery, the patient presented to the emergency department after four days of painless knee swelling. The patient decided to seek medical treatment only after developing subjective fevers. In the emergency department the patient was noted to have a significant effusion and his incisions were well-healed without erythema or drainage (Figure 1). He demonstrated pain less active and passive knee motion from 0-90 degrees, limited secondary to the large effusion. He was a febrile throughout his hospital stay, with an oral temperature of 99 0F on initial presentation.
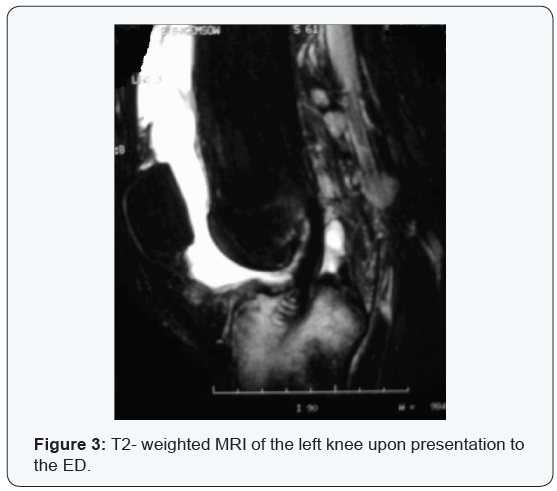
Aspiration had been performed by the Emergency Room physician prior to placing orthopaedic consult which revealed yellow, turbid fluid (Figure 2). The fluid analysis was significant for a differential of 117,000 white blood cells in aspirate, with no organisms on Gram stain. Peripheral blood tests and complete blood count revealed: WBC: 9.8; Neut-52.9, lymph-28.5, mono- 16.7, eo-1.7, baso-0.2. CRP 13, ESR: 33. Despite the relatively atypical presentation for a septic knee (lack of fever, absent pain, normal peripheral white blood cell count), the decision was made to proceed with a formal irrigation and debridement of the knee due to the size of the effusion and the elevated synovial white blood cell count. The patient’s father reported a recent history of Lyme disease, so Lyme titers were drawn for the patient prior to surgery. Additionally, an MRI was obtained while waiting for an available operating room to determine if there were any bony changes consistent with osteomyelitis or any loculated fluid collections that should be addressed during debridement. The MRI demonstrated a large effusion, no obvious synovitis, an intact ACL graft with no significant graft edema, and a large area of tibial edema (Figure 3).
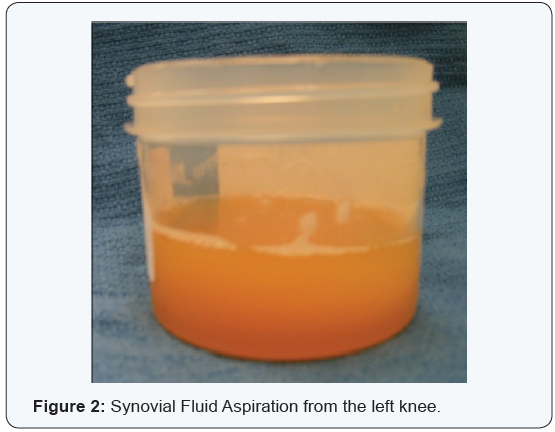
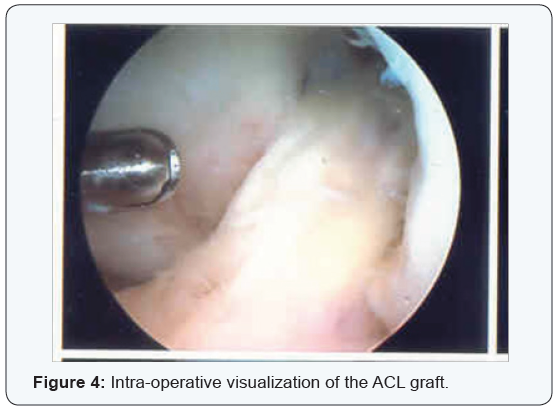
The patient was taken to the operating room several hours after presentation to the emergency room for an arthroscopic irrigation and debridement. Exam under anesthesia revealed a stable knee examination, with a re-accumulation of a large knee effusion. Approximately 90 mL of yellow, turbid fluid was aspirated prior to the start of the case and was sent for cultures, cell counts, crystal analysis. Additionally, multiple synovial biopsies and tibial bone biopsies were obtained. Arthroscopic evaluation showed healed meniscal tears, minimally inflamed synovium, turbid synovial fluid, and an intact and synovialized ACL graft (Figure 4). No articular cartilage damage was noted. After a thorough synovectomy and lavage with 9 liters of sterile saline, a drain was placed in a superior lateral portal and intravenous broad-spectrum antibiotics were continued while awaiting fluid culture and sensitivities to finalize.
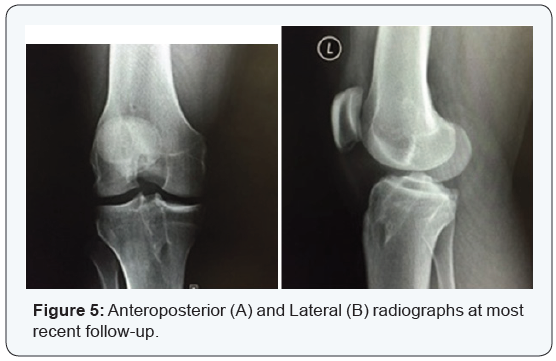
The intra-operative aspiration was negative for crystals and there were no organisms seen on gram stain, however a large inflammatory response with multiple white blood cells was noted on the microscopic examination. Lyme titers later revealed evidence of acute Lyme disease and the patient was transitioned to oral Doxycycline antibiotics as per the recommendations of the infectious disease consultant, with the typical regimen of four weeks of total treatment. At final five-year follow-up the patient had returned to full activity, and was back to playing rugby without complaints. On subjective outcome measures at 60 months, the patient had a Lysholm score of 99, and Tegner activity level of seven. Plain radiographs show no evidence of early arthritis, osteophytes, or joint space narrowing (Figure 5).
Discussion
Lyme disease is the most common tick borne illness in the United States, with its greatest prevalence in the Northeast, the Great Lakes area, and the Pacific Northwest. Late stage Lyme disease can typically affect the large joints, with the knee being most commonly affected [8]. There is often difficulty in diagnosing Lyme arthritis, with the diagnosis made on initial presentation in less than 20% of children [6]. There is similar difficulty in diagnosing Lyme in adults because the time course of symptoms and resolution varies patient to patient [9]. The diagnosis of Lyme disease or arthritis is dependent on clinical suspicion and obtaining the appropriate diagnostic tests. Frequently there is no history of a recent tick bite [10].
While a patient with Lyme arthritis may have an effusion, there are no specific radiographic criteria. Osseous changes, such as subarticular cysts and osteophytes have been noted, although they maybe incidental [9]. To date, diagnosis of Lyme disease via tissue or fluid culture has been unsuccessful; however polymerase chain reaction (PCR) of synovial fluid for B. burgdorferi DNA has a sensitivity of 80 to 85% [9]. The gold standard of Lyme disease diagnosis is dependent on visualization of antibodies to the causative spirochete by serum enzyme immunoassay (EIA), followed by Western immune blot confirmation, which can take up to a week [6].
In a retrospective study of 55 patients, untreated for Lyme disease, prior to antibiotic treatment was established 11 had no musculoskeletal symptoms after the resolution of bull’s eye rash, ie. Erythema chronicum migrans. Forty patients had joint involvement of some type. Arthralgias alone were seen in only 10 patients. These patients had brief episodes of pain in joints, and tendons that were migratory with a mean onset of 2 weeks after the onset of the rash Arthritic syndromes were seen in only 34 of the 55 patients that predominately affected the knees, with only seven patients developing large knee effusions [9]. Therefore, it is important to keep Lyme in the differential diagnosis of knee swelling even without associated musculoskeletal complaints.
Current literature regarding septic arthritis after ACL reconstruction is sparse, consisting of case reports of infection from a variety of organisms [11]. To our knowledge B. burgdorferi infection following an ACL reconstruction has not been reported. Patients with a typical septic arthritis after ACL reconstructive surgery present with fevers and an acutely swollen, painful joint. Knee motion is limited with an associated effusion, erythema, and warmth. Occasionally there will be drainage from the surgical incisions. Conversely, the patient in our case had an atypical presentation with no warmth or erythema of the knee and no pain with knee motion. While the patient reported subjective fevers at home, there were no documented fevers in the hospital.
There are many risk factors for septic knee arthritis after arthroscopic ACL reconstruction. Prior knee surgery, concomitant surgical procedures during ACL reconstruction, perioperative wound contamination, allograft usage, and presence of intra-articular foreign bodies are potential risk factors [12]. Other risk factors for infection after arthroscopic procedures include patient age greater than 50 and prolonged tourniquet time greater than 60 minutes [1]. It is reported that 53% to 75% of patients who developed septic arthritis after ACL reconstruction have had previous surgery on the same knee [12]. There are several conduits of potential infection after ACL reconstruction, including the arthroscopic portals, as well as the tibial and femoral tunnels. Usually, the tibial tunnel incision is the most common site for deep wound infection, associated with septic knee arthritis after ACL reconstruction due to its relatively superficial anatomic location [10].
Other potential niduses of infection include any hardware such as cannulated screws, suture material, or mensical arrows inside the joint. Williams et al published a case series of 7 patients (0.3% of cases) with postoperative intra-articular infections after ACL reconstruction [13]. Six of the 7 patients had a concomitant procedure in addition to the ACL reconstruction. Four of the seven patients had acute infections, between 2 weeks and 2 months the remaining 3 patients developing infection between 2 weeks to 8 weeks. Treatment was performed with arthroscopic irrigation, debridement, synovectomy, and graft removal in 4 patients, followed by a prolonged course of culturespecific intravenous antibiotics [13]. Mean follow-up of 29 months, mean knee extension was 0 degree, and mean knee flexion was 122 degrees [13]. Eight-six percent of patients had minimal to no pain in their operative knee, and were satisfied with their results.
The primary goals in managing any septic arthritis after ACL reconstruction are to protect the articular cartilage and the graft [2]. The inflammatory response in a typical septic arthritis causes synovitis and chondrolysis [12]. A thorough irrigation, debridement, and aggressive synovectomy is important to lower the number of bacteria in the infected joint, as well as to minimize the common complications of osteoarthritis, osteomyelitis, and arthrofibrosis [2]. Arthroscopic irrigation and debridement is associated with a shorter postoperative recovery time with less morbidity than a formal open knee arthrotomy [2]. A survey of sixty-one Sports Medicine Fellowship program directors showed that 85% of the surgeons would use culture specific intravenous antibiotics with an arthroscopic irrigation and retention of the graft in the patellar tendon autograft recipient, and 64% would do the same if the patient had received an allograft. If the graft were removed, revision was favored after 6 to 9 months [7]. Our patient’s atypical presentation with painless knee motion, lack of objective fevers, and overall benign appearance led us to favor graft retention prior to surgery. Once in the operating room, the benign appearance of the joint and integrity of the ACL graft itself at the time of arthroscopy confirmed our decision.
While our patient did not have a typical presentation of septic arthritis, the elevated synovial WBC as well as the un-explained effusion led us to proceed with an arthroscopic irrigation and debridement. Patients with Lyme arthritis may not present with the fevers or joint pain characteristic of bacterial septic arthritis, but can have elevated synovial leukocyte counts, as well as elevated serum WBC, ESR, and CRP levels [6]. Compared to a typical bacterial septic arthritis, Lyme arthritis has a more indolent progression. Unlike bacterial septic arthritis, which can leads to joint destruction very quickly, Lyme disease does not cause chondrolysis in the acute setting. However, if left untreated Lyme Arthritis can develop long term arthritis in 50- 60% of patients [8]. B. burgdorferi spirochetes can induce an inflammatory response in synovial tissues that is very similar to the presentation of an acute septic arthritis [8].
Unlike common pathogens Staphylococcus aureus or Streptococcus pyogenes, B. burgdorferi does not produce proteases to digest collagen and other proteins of articular cartilage. Research in animal models, suggests that joint damage due to B. burgdorferi is caused by host inflammation and is induced by matrix metalloproteinases 1, 3, and 13, similar to Rheumatoid arthritis [8]. Further complicating the diagnosis is that one has to rely on PCR, as it is not possible to culture B. burgdorferi from synovial fluid [8]. In the setting of recent ACL reconstruction without the ability to rapidly distinguish between Lyme arthritis and bacterial septic arthritis, the decision was made in our patient to urgently irrigate and debride the joint. With an acutely swollen joint and elevated synovial leukocyte count, and the fact the patient’s father recently was treated for Lyme disease, we proceeded to the operating room with presumptive diagnosis of Lyme arthritis.
It is believed that early therapeutic intervention, infection with a low-virulence organism, graft retention, and early physical therapy are essential for successful treatment in the post-ACL joint infection [10]. An algorithm for treatment was outlined by Williams et al in their retrospective study involving seven patients after ACL reconstructive surgery with a postoperative deep infection [14].
If laboratory studies and aspiration indicate a likely septic arthritis, immediate irrigation and debridement of the joint and incisions was recommended. The authors felt that graft removal was a decision left to the discretion of the surgeon, and could be performed later if there are persistent signs of infection after the first irrigation and debridement. Post-operatively their recommendations included six weeks of parenteral antibiotics based on the culture results. In patients who underwent graft removal, these authors recommended repeat ACL reconstruction only after a one year symptom free interval in high level athletes with a 2+ pivot shift and symptomatic instability [11]. Typically, Lyme arthritis is treated successfully with oral or intravenous antibiotic regimens initially for 4 weeks. Doxycycline at a dose of 100mg BID, it the usual agent of choice. Other options are amoxicillin, azithromycin, cefuroxime-axetil, clarithromycin.8 Our patient was treated with an immediate irrigation and debridement, followed by 4 weeks of oral doxycycline.
Ultimately, our patient achieved a successful outcome with full return to sport and activities. However, many other authors have reported suboptimal results in treating patients with septic arthritis after ACL reconstruction. McAllister et al. [5] reported on four cases of postoperative septic arthritis treated with immediate arthroscopic lavage, open incision, drainage of associated wounds, debridement with graft retention, and treatment with intravenous and oral antibiotics [5]. These cases were evaluated three years after surgery. Three of the patients had an autogenous patellar tendon graft; the other had a quadruple-stranded semitendinosus autograft. An average of 2.75 procedures was necessary to sterilize the joint. Although these patients had similar results in terms of instrumented knee laxity and isokinetic strength deficits when compared to patients with uncomplicated ACL reconstructions, they had lower Lysholm scores and International Knee Documentation Committee (IKDC) scores. The authors attribute the poorer outcomes to articular cartilage damage secondary to the infection, which they noted on radiographs and MRI [5]. A group of patients that underwent graft removal, in addition to arthroscopic lavage and use of intravenous antibiotics, was reported on by [4]. Of the seven patients that had the graft removed, four subsequently had repeat reconstructions. This occurred within six weeks of completion of an extended antibiotic course. At follow-up twenty-one months after surgery, range of motion was full and symmetric, the KT-1000 arthrometer detected 3mm side to side difference, and the modified Lysholm score was similar to those with an uncomplicated course [2]. These results stand in contrast with those in the graft retention series presented by McAllister [15]. The fact that our patient did comparatively well likely is a result of the indolent nature of the infecting organism, as even 4 days after the onset of symptoms there was no chondral damage noted. This key distinction of B. burgdorferi is important when considering treatment of these patients, as graft removal may be beneficial in the setting of bacterial infection, but may not play a significant role in patients with Lyme arthritis.
In summary we report on a patient who underwent successful treatment for Lyme arthritis after ACL reconstruction. Because of the atypical physical exam findings, the history of the patient’s father recently treated for Lyme disease, and that the patient resided in an area with a high prevalence of Lyme infections were all important clues to raise the suspicion of Lyme disease. Even though B. burgdorferi does not produce proteases to digest collagen and other proteins of articular cartilage, joint damage due to B. burgdorferi can occur due to the host inflammatory reponse [8]. Therefore, in the setting of recent ACL reconstruction without the ability to rapidly distinguish between Lyme arthritis and bacterial septic arthritis, the decision should be to urgently irrigate and debride the joint. Furthermore, without evidence of other cases in the literature, we continue to recommend aggressive treatment for any suspected case of infection in the post-operative ACL reconstruction patient.
Conclusion
If the patient’s appearance is somewhat atypical and they reside in a region where Lyme disease is prevalent, we also encourage serologic testing for B. burgdorferi. This should be followed by organism specific antibiotics at the recommendation of an infectious disease specialist. In our opinion graft retention is at the discretion of the surgeon but should be influenced by duration of symptoms, time from initial reconstruction, other co-morbid factors such as diabetes, as well as the appearance of the joint and graft itself at the time of surgery.
To Know More
About Orthopedics and
Rheumatology Open Access Journal Please click on:
For more about Juniper Publishers Please click on:



Comments
Post a Comment