Juniper Publishers - Fractures of the Proximal Third Tibia Treated With Intramedullary Interlocking Nails and Blocking Screws
Orthopedics and Rheumatology Open Access Journal
Abstract
Background: Internal splint age of proximal metaphyseal tibial fractures has gained acceptance as a method of early stabilization of such injuries. Intramedullary nailing is a challenging procedure .This study tries to evaluate treatment outcomes of closed reduction and intramedullary nailing with the aid of blocking screws to maintain the reduction and stabilize theses injuries.
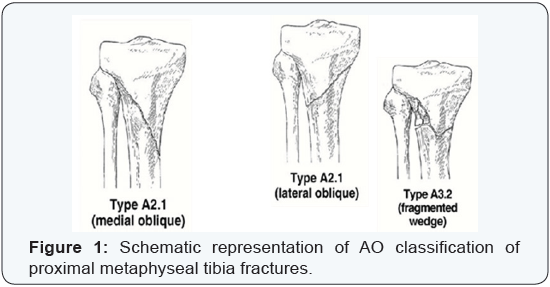
Patients and Method: Thirty patients (23 males and 7 females) with proximal metaphyseal tibial fractures were treated and followed from June 2010 and February 2014 (44 months) with average 19 months. Age ranged between 23 to 55 years (average, 38 years). According to A.O. Classification 13 cases were Type A 2.1, 9 cases were Type A 2.1 (II), and 8 cases were Type A 3.2. Seven cases were open fractures and according to Gustilo Anderson classification 4 cases were Grade (I), 3cases were Grade (II). All cases were treated by interlocking intramedullary tibial nailing assisted by the use of blocking screws technique.
Results: The results had been evaluated through the following parameters: (pain, union, malunion, infection, range of motions, walking capacity, extension lag, knee stability and implant and technical failure. All cases had been united. Excellent alignment obtained in 27 fractures (90%). Knee and Ankle joints range of motions were equivalent to the unaffected side in 25 patients (82%). Two patients got superficial wound infection (2.7%). The final functional results were evaluated through modified Karlstrom-Olerud Score and we get: Excellent: 20 cases (66.7%), Good: 7 cases (23.3%), Satisfactory: 2 cases (6.7%) and Poor: 1 case (3.3%).
Discussion: Intramedullary nailing of proximal tibial fracture is a load sharing procedure, sparing the extraosseous blood supply, avoids additional soft-tissue dissection, thereby minimizing the risk of postoperative complications. Also, it reduces the length of hospital stay and costs, enables early mobilization and achieves satisfactory outcomes. However; it is a technically demanding procedure and may result in malalignment. Our aim is evaluating the clinical use of Pollar screws (blocking screws) as a supplement to stability fixation of these fractures with statically locked intramedullary nails.
Conclusion: Utilizing intramedullary interlocking nailing supplemented with blocking screws to aid in stabilizing proximal tibial fractures whether closed or open is a good method of treatment. The high proportions of excellent and good results in our series confirm that this technique is equal to other known methods of fracture fixation.
Keywords: Intramedullary nail; Proximal tibia fracture; Blocking screws
Introduction
Proximal tibial fractures considered a more challenging injury. The goals of treating these fractures are: achieving bony union, restoring soft tissue vitality, preventing infection and instituting early joint motion and muscle rehabilitation [1]. A wide variety of nonsurgical and surgical methods of treatment are available. They can be used in isolation or in interesting combinations involving two or more methods, depending on peculiarity of fracture, the age and health of the patient and other imperatives that might be imposed by associated injuries. Although intramedullary nailing becomes a standard biological procedure for managing diaphyseal fractures of long bones; it is still a debatable issue regarding its use in proximal tibial fractures [2].
Patients and Method
Thirty patients with proximal tibial fractures were treated and followed between June 2010 and February 2014 (44 months) with average 19 months. There were 23 males and 7 females. Age ranged between 23 to 55 years (mean, 38years) years. In 17 cases (56.7%) fracture was due to road traffic accident, 11cases (36.6%) due to work related injuries, and in 2cases (6.7%) due to sport injuries. Seven cases were open (4were Grade (I) and 3 were Grade (II) according to Gustilo-Anderson classification [3].
According to the A.O. Classification: 13 cases were Type A 2.1 (medial oblique), 9 cases were Type A 2.1 (II) (lateral oblique), and 8 cases were Type A 3.2 (fragmented wedge) (Figure 1).
Exclusion criteria involved pathological fractures, adolescent patients below 17 years old, patient with previous diaphyseal fracture, non-united fractures and fractures extending to the articular surface. Ethical clearance was obtained from the institutional ethics committee and informed consent forms from all patients were received. All cases were stabilized by intramedullary interlocking tibial nails (8-10 mm of diameter and 34 to 38 cm long).
Surgical technique
Length and width of nail was provisionally determined preoperatively. The proper nail assembled to the Distal Locking Target Device to adjust distal locking screws position. All patients had been operated-upon under general anesthesia and were placed supine on a radiolucent table. For open fracture cases; thorough irrigation was done utilizing 2-4 liters saline solution. All contaminated, devitalized soft tissues were excised. Broad spectrum antibiotic was given (3rd generation cephalosporin, 2 gm IV) just before induction and continued for 2 weeks. The knee poisoned in 90 degree flexion. A longitudinal incision about 4 cm was made from the inferior pole of the patella just medial to the patellar tendon, and extended distally. The infrapatellar fat pad was identified and its insertion into the insertion into the proximal tibia was sharply incised transversely allowing its retraction superiorly for exposure of the proximal tibial ridge.
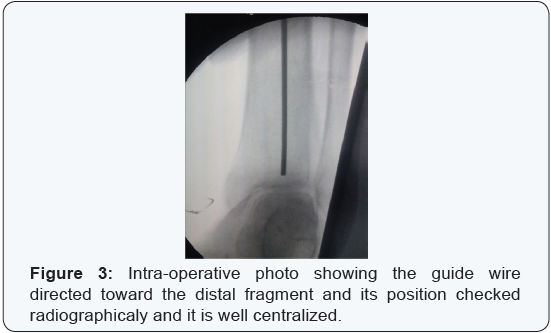
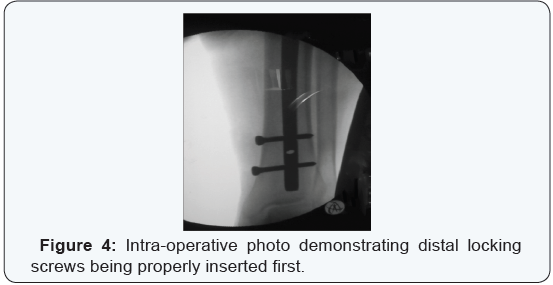
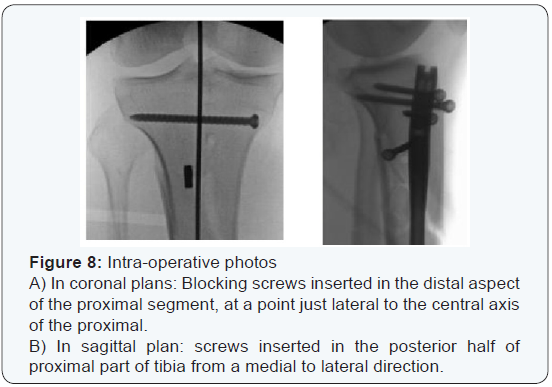
The entry point of nail detected and opened using a curved Awl. Guide-wire passed through medullary canal down to level of the fracture site under direct vision (in cases of Open fractures) while utilizing image intensifier (in cases of closed fractures) (Figure 2). The fracture was manipulated manually or by using percutaneous clamp to achieve reduction. The guide wire then was directed toward the distal fragment and its position was checked again radiographicaly for further confirmation (Figure 3). Blocking screws were inserted percutaneously. The anteroposterior screws were inserted in the distal aspect of the proximal segment, just lateral to the central axis of the proximal tibia. The sagittal plan screws placed in the posterior half of the proximal part of the tibia from a medial to lateral direction. The chosen nail attached to insertion jig and driven over the guide wire through the medullary canal. Distal locking Target Device assembled to the jig and distal locking screws were inserted first (Figure 4), then the proximal ones (Figure 5). Wounds closed and dressed.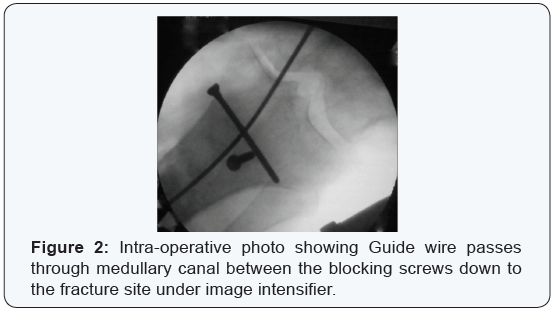
Post-operative regimen
Wounds dressed every other day. Patients were mobilized on first postoperative day where knee and ankle joints exercises started. Partial weight bearing was encouraged for those who had no other associated injuries prohibiting walking. Patients were allowed for touch weight bearing on first post operative day, half weight bearing for three weeks then full weight bearing when callus was seen on follow-up X-Rays. Supervised physical therapy was initiated for thigh muscles strengthening and knee range of motions exercises.
Results
All patients agreed to present our timetable of follow up until they get their fractures united and started pain free full weight bearing. The patients were followed up postoperatively at 2 and 4 weeks, 3 months, 6 months, and 1 year. The mean length of hospital stay was 6 days (range 2-19days). The results of the study had been evaluated through: union of fracture, ranges of motion of both knee and ankle joints, alignment of fracture,occurrence of infection, degree of knee pain, walking capacity, extension lag and stability of the knee joint. All cases had been united. Average union time was 15 weeks in 12 patients (40 %), from 16-20 weeks in 15 patients (50%) from 21-28 weeks in 3 patients (10 %). There were no cases of nonunion. Knee and ankle joints range of motions were measured using Goniometer. In 25 patients (83.3%) it was equivalent to the unaffected side but 3 patients (10%) got knee joint flexion restricted to about 85°, whereas 2 patients (6.7%) had 10- 15° restricted range of ankle motions. Accuracy of reduction and final alignment were evaluated via assessing the immediate postoperative and the final follow-up radiographs.
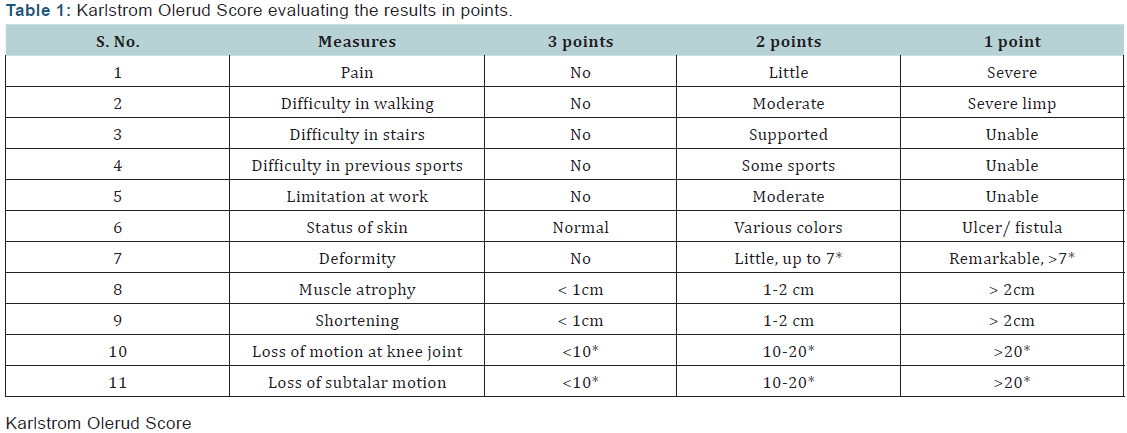
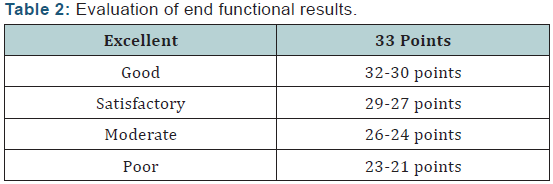
Only 3 patients (10%) had malalignment. (Two of them had 10° and 40° varus angulation respectively and one case had 10° valgus). Two patients got superficial wound infection (6.7%). One of them got wound infection in the distal screw entry sites and one patient got wound infection in the proximal nail entry sites and both responded well to antibiotics. Regarding knee pain, it was assessed after complete union of fractures. Twenty- Two patients (73.3%) denied knee pain with any activity whereas 8 (26.7%) patients had at least moderate knee pain after vigorous activity. At last follow-up 28 patients were able to walk freely without assistance (cane or crutches), while 2 patients used walking aid during free walking. Two patients had extension lag about 100 while 3 patients had less than 15o lag the rest of patients (25 patients) had no extension lag. Only one patient had moderate knee instability. In our series No case of neither implant nor technical failure developed. The overall final functional results had been evaluated using Modified Karlstrom- Olerud Score (Tables 1 & 2).
Discussion
Controversy still remains regarding the use of IMN as a definitive management of proximal third tibial fractures [4,5]. Historically, these injuries have been notoriously difficult to fix and maintain without early failure in some reported series [6]. Malunion rates have been reported to be high and several earlier series offered high rates of fracture failure, typically into an apex anterior and valgus position [7,8] (Figure 6). The natural bony anatomy and muscular attachments of the proximal tibia offers the perfect set up for a number of common deformities after fracture with subsequent malalignment during IMN placement. These are due to muscular stresses via tendinous attachments [9]. The dynamic forces of the patellar tendon pull the proximal fragment into an apex anterior angulation, whereas the attachment of the pes anserinus causes valgus stress on the same fragment (Figure 7).
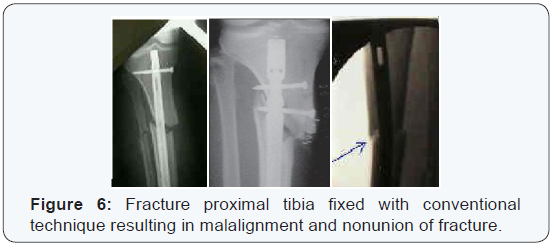
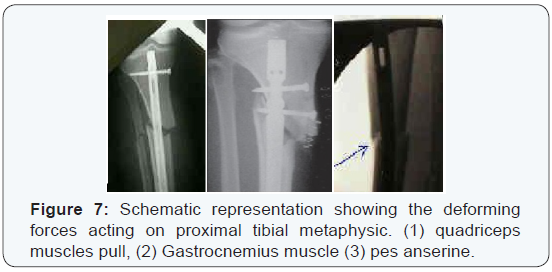
These forces; in addition to the capacious medullary canal at this level, create the potential for improper reduction and suboptimal nail placement during nailing with conventional techniques for IMN of proximal third tibial fractures with the knee hyper flexed [10]. Early frustrated results disappoint surgeons from using of IMN for proximal third tibial fractures. However, with continued research and proper understanding of the specific anatomy and deforming forces surrounding the proximal tibia; several technical modifications evolved that can maintain reduction, restore native anatomy and consequently improve outcome results. The accompanied studies exhibit high rates of union and low resultant deformities which renewed the interest of IMN usage for proximal third tibial fractures [11]. Our study outlines some of technical tricks and management pearls available for treating proximal third tibial fractures via IMN, with blocking screws in order to regain the normal mechanical axis, proper length and neutral rotation [12].
In our series; the coronal plan blocking screws are inserted in the distal aspect of the proximal segment, at a point just lateral to the central axis of the proximal tibia (not the central axis of the fracture); hence the nail passes medial to the blocking screws. In the sagittal plane; blocking screws are placed in the posterior half of the proximal part of the tibia (just posterior to the central axis) from a medial to lateral direction allowing the nail to remain to the anterior cortex as it is inserted down the canal (Figure 8). The pollar screws which had been used to supplement intramedullary nailing of tibial fractures would improve stability of fixation and minimize the development of angular deformity [13].
From mechanical point of view; Pollar screws function through the principle of 3-point fixation. By this it would abolish all forces exerted by muscles and ligaments on the proximal tibial fragment. Also, it lessen the path via the metaphysic [7,13]. We revised some studies utilizing same technique of fixation [10,11,13-15]. The prolonged period of follow-up which was not issued by some studies gave us a chance to predict even minor complications and those shortcomings that require very long period of follow-up [15]. The average age of patients was 34.4 years. This age group needed to return back to work as soon as possible, so early mobilization is mandatory. Union could be detected clinically when the patient is walking without pain on the operated leg with full weight bearing and on radiological examination bridging bone callus on at least three of the four cortices in the Antero-posterior and lateral views is visible.
No cases of non-union developed in our series and these results are more or less coincident with the results of other studies [14,16,17]. Malunion was analyzed at the time of union as the axis deviation between the proximal and distal fragment at the level of the previous fracture, on the anteroposterior and lateral x- rays. It was measured on long x-ray films and in some cases CT scanogram was utilized. Avoidance of this complication prohibits the development of joint pain and degenerative joint disease [18]. It was reported in 3 cases (10%); two of them were due to technical defects and the third case showed sever comminution and at the same time the patient bear weight early without protection as recommended by many authors [5]. Although Seven patients (23.3%) in this study have open fractures, there is a concern that performing an extended incision (which requisite arthrotomy) may lead to pyarthrosis.
Despite this concern, just one patient with open injury developed superficial infection. There was no cases of deep infection and this may be attributed to proper management of open fractures and preservation of soft tissue envelop around the fracture ends in addition to adequate antibiotic coverage [19,20]. Range of motions of knee and ankle joints as a key for evaluating efficiency of the technique was evaluated after complete union of fracture. There were 25 cases (83.3%) regained full range of motions for both knee and ankle joints and this attributed to the early rehabilitation of the patient’s joints In 5 cases (16.7%) the range of motions of knee and ankle joints were affected. All of them related to open fractures (3 Grade (I) and 2 Grade (II) which explains that the more the soft tissues damage the more the delay of patient recovery which in turn affecting the nearby joints range of motions [21].
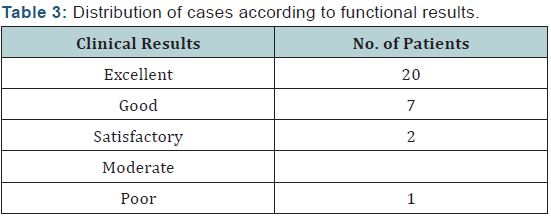
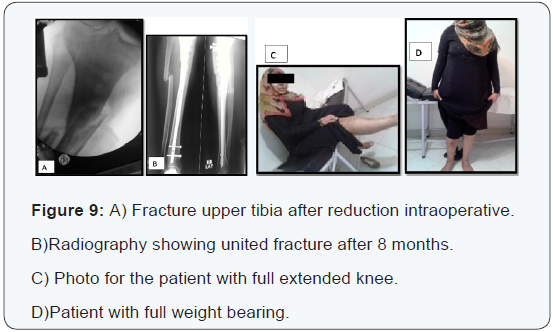
The overall functional results were evaluated utilizing Modified Functional Evaluation System by Karlstrom-Olerud Score [22]. They were as follows: Excellent: 20 cases (66.7%), Good: 7 cases (23.3%), Satisfactory: 2 cases (6.7%) and Poor: One case (3.3%) (Table 3). Giving details of surgical technique as regard point of nail insertion, semi extended position during nailing, polar screws to avoid deforming forces acting on the proximal and distal fragments all are technical challenge to attain perfect reduction and finally good results [11,23]. In contrast to open reduction and internal fixation, intramedullary nailing can be performed initially on the first or second day of admission (Figure 9) presenting a female patient 25 years with open fracture proximal right tibia (A), after using the mentioned technique; the fracture fully united by 8 months (B), patient has full knee extension (C) and can put full weight bearing (D).
Conclusion
The results of the study share the idea that tibial nailing of proximal metaphyseal fractures aided by blocking screws being a suitable procedure. The advantages include being a familiar technique for fixing tibial shaft fractures; allows osteosynthesis under biological aspects; no need to open the fracture site; soft tissue dissection is not necessary; and the blood supply is spared. It enables symmetric, dynamic and load-sharing fracture stabilization without the need to restrict joint motion.
To Know More
About Orthopedics and
Rheumatology Open Access Journal Please click on:
https://juniperpublishers.com/oroaj/index.php
For more Open Access
Journals in Juniper Publishers please click on:
https://juniperpublishers.com/index.php
For more about Juniper Publishers Please click on:
https://juniperpublishers0.wixsite.com/juniperpublishers


Comments
Post a Comment