Juniper Publishers - Outcome of Endoscopic Calcaneoplasty in Insertional Achilles Tendinopathy with Retrocalcaneal Bursitis. A New Prospective Study
Orthopedics and Rheumatology Open Access Journal
Abstract
Introduction: The aim of this study in to analyze the outcome of Endoscopic Calcaneoplasty Technique for the treatment of Insertional Achilles Tendinopathy with Retrocalcaneal Bursitis.
Methods: This prospective study consists of 6 patients (3 men, 3 women) with mean age of 44.3 years who were operated by a single surgeon from March to November 2014. The bone cutter shaver was used to remove sufficient amount of inflamed retrocalcaneal bursa and superior part of calcaneum under fluoroscopy guidance. All patients were discharged on the following day and allowed weight bearing as tolerated. American Orthopedic Foot and Ankle Society (AOFAS) score, SF-36 health survey score and Ogilvie-Harris score were documented at 3rd and 6th months follow up.
Results: All patients were followed up for at least 6 months. AOFAS scores showed significant improvement at 3rd and 6th months with p value of 0.028. SF-36 scores showed overall significant changes for physical functioning (p=0.04), physical role limitation (p=0.035), emotional wellbeing (
Conclusion: Endoscopic calcaneoplasty is a safe and effective technique for the treatment of Insertional Achilles Tendinitis with Retrocalcaneal Bursitis.
Keywords: Endoscopic; Calcaneoplasty; Achilles Tendinitis; Fluoroscopy; Bursa
Abbreviations: AOFAS: American Orthopedic Foot and Ankle Society; SF: Short Form; SPSS: Statistical Package for the Social Science; ESWT: External Shockwave Therapy
Introduction
Achilles tendinopathy is a common hind foot disorder which affects both the active and non-active population. It’s occurence among Asians has shown an increasing trend due to their active involvement in sporting activities but limited literature is available documenting on Achilles tendinopathy. It can be classified as insertional and non- insertional tendinopathy [1]. Insertinal tendinopathy is responsible for 20% to 25% of total Achilles tendon related disorders [2] and usually associated with retrocalcaneal bursitis. Insertional Achilles tendinopathy is a clinical syndrome consisting of pain, swelling and impaired performance. The pathology is located at the insertion of Achilles tendon on the postero-superior part of calcaneum and commonly associated with formation of bone spurs and calcifications of Achilles tendon.
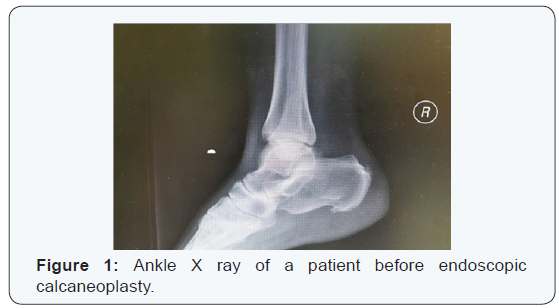
Insertional Achilles tendinopathy is purely a clinical diagnosis. Patients presents with complaint of pain, appear at the beginning and ending of walking session, stiffness and occasionally swelling of the hind foot. Examination findings include visible swelling, tenderness at postero-lateral aspect of the calcaneum and a palpable bony spur. Imaging like plain radiography and MRI can be used to support the diagnosis and exclude the differential diagnosis. Plain radiography may show ossification, a bone spur at the tendon’s insertion or radio-opacity of the retrocalcaneal recess. Meanwhile, MRI may reveal any bone formation or hyper intense signal at tendon insertion or retrocalcaneal recess.
The scientific evidence of the etiological factors is limited. The suggested pathophysiology is excessive loading during exercise or recurrent microtrauma leading to tendon damage [3]. The risk factors can be either intrinsic or extrinsic. Intrinsic factors include tendon vascularity, gastrocnemiussoleus dysfunction, age, gender, obesity, hypertension, diabetes mellitus, dyslipidemia, pes cavus and lateral ankle instability [4]. Meanwhile, extrinsic factors are changes in training pattern, poor technique, previous injuries, footwear and training on hard, slippery or slanting surfaces [2,5].
This disorder is initially treated with non-operative treatment. Patients are advised for complete or modified rest and correction of possible intrinsic or extrinsic risk factors that may contribute to pain. Adequate analgesia, local injection of sclerosing agents, physiotherapy to strengthen the triceps surae muscles and orthotic treatment like shoes change or heel lift have shown some symptomatic improvement [6]. McGarvey et al. [7] have shown that 89% of their patients improved with nonoperative treatment.
Surgical intervention is recommended for failed nonoperative treatment. The surgical principle involves removal of the inflamed bursa, thickened synovium and resection of postero-superior part of calcaneum. There are many surgical options available such as open and endoscopic method with good to excellent outcomes. A recent systematic review by Wiegerinck et al. [8] has concluded that endoscopic surgery is better compare to open intervention. This study is conducted to analyze the outcomes of endoscopic calcaneoplasty in a single operating centre within the Asian population. American Orthopaedic Foot and Ankle Society (AOFAS) hind foot scoring system, Short Form (SF 36) Health Survey and Ogilvie Harris scores were used to evaluate the patient’s outcome.
Materials and Methods
This prospective study covers 9 patients (4 men, 5 women) with mean age of 44.3 years who were operated by a single surgeon from March to November 2014. Patients are selected based on the criteria of failed conservative management for a minimum of 4 months, declared fit for operation by anesthetist and have given consent for operation. Persisting pain and difficulty in walking were the main indications for operation.
History taking and examinations were repeated to establish the diagnosis of Insertional Achilles Tendinopathy. Plain radiography and MRI were done for all the patients to confirm the diagnosis, exclude the differential diagnosis and ensure the integrity of the Achilles tendon. Written consents were obtained from all the patients for the operation. 3 patients refused surgery just before the scheduled date due to social reasons.
All the operations were done under general anesthesia.
Prophylaxis dose of Intravenous Cefuroxime 1.5g was given to the patient at the time of induction. The patients were positioned prone with feet lying at the edge of the operating table. The affected leg was raised slightly with rolled towel.
Area of interest was painted with Povidone Iodine and draped. Thigh tourniquet was inflated after exsanguination of the leg using crepe bandage. The degree of dorsiflexion of the foot is manipulated by using the surgeon’s body against plantar surface of the foot.
Endoscopic calcaneoplasty uses medial and lateral portals. Lateral portal was created by making a small vertical skin incision at the level of superior part of calcaneum lateral to Achilles tendon. Blunt trocar was used to reach the retrocalcaneal space and is replaced with 4.5-mm arthroscope shaft at the angle of 30°. Meanwhile, medial portal was created by using a spinal needle as a guide at the superior part of calacaneum medial to Achilles tendon. Stab incision was made and Kelly’s forceps were used to reach the retrocalcaneal space. Bone cutter shaver was introduced from medial portal and once placement was confirmed by using arthroscopy, the inflamed bursa and superior part of the calcaneum were removed using shaver. Sufficient amout of calcaneum was removed by manipulating ankle joint into dorsiflexion and plantarflexion position with the help of fluoroscopy. Cutter surface of shaver was always placed facing the calcaneum to protect the Achilles tendon [9].
The skin was closed with non-absorbable sutures and compression dressing was done. All the patients were discharged on the following day of operation after reviewing post-operative plain radiographs. Patients were advised for range of motion exercises and weight bearing as tolerated. Wounds were inspected on day 3 and sutures were removed at 2 weeks. All the patients were followed up at 1, 3 and 6 months following operation.
The American Orthopaedic Foot and Ankle Society (AOFAS) hind foot scoring system, Short Form (SF 36) Health Survey and Ogilvie Harris scores were calculated pre- and postoperatively. Each patient was assessed by two independent reviewers for pre and postoperative scoring and average scores were taken for each follow up. Patients also were asked whether will undergo the same operation if his or her contralateral foot is affected. Statistical Package for the Social Science (SPSS) was used to analyze the data and calculate the p value.
Results
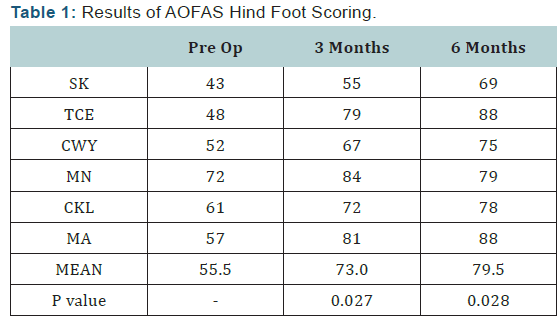
All the patients were followed up for at least 6 months. For each visit, all the patients were re-examined and assessed for AOFAS Hind Foot Scoring, SF-36 scoring and Ogilvie Harris scoring. Pre-operative and post-operative scores at 3 months and 6 months were calculated and compared as shown in the tables below (Tables 1-3). The AOFAS Hind Foot Scoring is based pain (40 points), function (50 points) and alignment (10 points). The mean AOFAS score improved from pre-operative score of 55.5 (range, 43-72) to post-operative score of 73.0 (Range, 55- 84) at 3 months and 79.5 (range, 69-88) at 6 months. Wilcoxon signed rank analysis showed significant AOFAS scores with p values of 0.028 at 3 months and 6 months. Only one out of six patients had daily pain at 6 months follow up and could be due to scar tenderness.
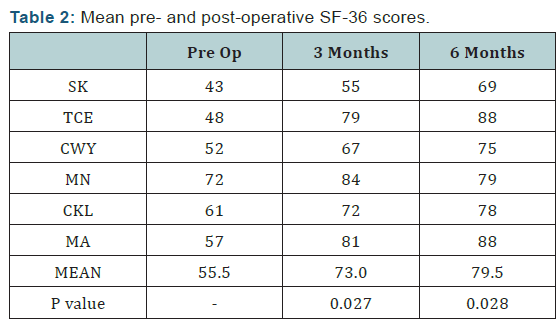
The SF-36 Health Survey evaluates 8 parameters with the scores ranging from minimum of 0 to maximum of 100. Based on repeated measure ANOVA, average scores of SF-36 showed significant changes for physical functioning (p=0.04), physical role limitation (p=0.035), emotional wellbeing (p=0.005) and pain (p=0.003).
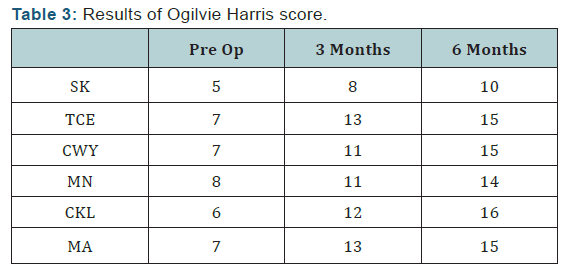
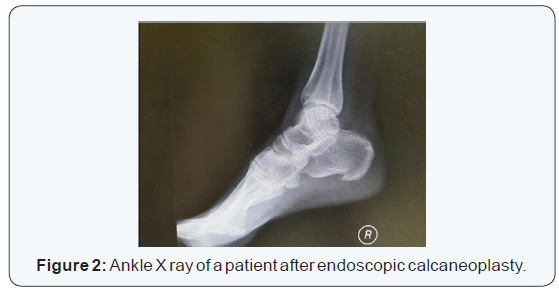
Ogilvie Harris scoring is based on clinical assessment with maximum score of 16. The results were scored as excellent (15 to 16 points), good (13 to 14 points) or unsatisfactory (<13 points). At 6 months follow up, 4 patients had excellent results, one had good result and one had unsatisfactory result. 5 out of 6 patients agreed for the same operation if contralateral foot is affected. All the wounds healed well and no incidence of infection was reported. Although all patients had improvement in all scores evaluated as compared to preoperative scores, one patient has persistent scar tenderness (Figures 1 & 2).
Discussion
Insertional Achilles Tendinopathy can be treated with or without operation and choice of treatment depends on patients. Non-active patients may choose non-operative treatment for a period of 4 to 6 months before deciding for operative treatment. Meanwhile, active patients like professional sportsman may directly opt for operation without non-operative treatment for early return to sports and work. A wide range of non-invasive and non-operative methods have been developed and modified to treat Insertional Achilles Tendinopathy. However, the success rate is inconclusive due to insufficient clinical evidence [10]. Surgical options are offered for failed non-operative treatment. Open and minimal invasive surgeries have shown excellent results but minimal invasive surgeries are gaining popularity among patients due to early work and sport resumption [11].
Non-operative treatment includes adequate rest of the Achilles tendon from excessive load and gradual muscle exercise to build the strength of the triceps surae muscles [12]. Patients are advised to avoid tight shoes and improvise their techniques in work and sporting activities [6,13]. Non-steroidal antiinflammatory drugs have only analgesic effect without any long term benefit [6,13]. Corticosteroid injections are being offered to patients by some centers but the safety of its usage in our center is outweighed by the complications. Adverse effects of using corticosteroid includes reduce strength of the tendon, thus precipitate tendon rupture [14]. None of the patients in our center was given corticosteroid injection. External shockwave therapy (ESWT) have shown high success rate when combined with eccentric exercises. Vulpiani et al. 2009 have concluded that ESWT has positive effect on the treatment of tendinopathy with long lasting improvement of pain [15].
Surgical options for Insertional Achilles Tendinopathy have changed tremendously in the past decade due to advancement of technology and increased social needs of patients. It can be divided into open and minimal invasive surgeries. Open calcaneoplasty used to be the gold standard of surgical interventions until minimal invasive surgery become available. Many literatures have reported the good outcome of open surgery. However, open surgeries are highly invasive, associated with many complications and patients need longer recovery time. Common complications associated with open surgery are surgical site infection, wound dehiscence, bad scars and rupture of Achilles tendon [16-18].
Study conducted by Chen CH et al. [17] on 19 patients (30 heels) who underwent excision of the posterior calcaneal tuberosity and bursectomy through a medial longitudinal incision with average follow up period of 6 years, 10% of the patients had persistent pain and 83% had residual pain for half to two years after operation. Meanwhile, Angermann et al. [18] reported the outcome on 40 patients (40 heels) who were managed by resection of the posterosuperior aspect of calcaneum through posterolateral approach. Results after an average of 6 years showed 50% of heels recovered, 20% were improved and 10% were worse among 37 patients who were allowed immediate weight bearing. Documented complications include one superficial heel infection, one hematoma and two cases of delay wound healing.
Advantages of endoscopic technique over open surgeries are short recovery time, rapid return to work and sports, small incision and good scar healing [19]. Van Dijk et al. [20] reported endoscopic calcaneoplasty in 2001. In this study, endoscopic calcaneoplasty was performed in 20 patients (21 heels). The average follow up was 3.9 years and one patient had fair result, 4 patients had good results and the remaining 15 patients had excellent results. Most of these cases are same day surgery and patients do not need to stay overnight. There were no surgical and post-operative complications. All the patients had short recovery time and quickly back to work and sports. Systematic review on surgical treatment of chronic retrocalcaneal bursitis has reported 12 open surgical technique trials and 3 endoscopy technique studies evaluating 547 procedures in 461 patients [21]. Patient satisfaction and complication rate favored endoscopic technique.
Studies reporting the outcome of endoscopic calcaneoplasty among Asian populations with Insertional Achilles Tendinopathy are very limited. Late presentations to hospital among Asians due to higher pain threshold and tendency to try out traditional treatment may affect the outcome of endoscopy calcaneoplasty. This study has shown a good outcome and can be used as reference for future research with larger sample size and longer follow up durations.
Conclusion
Endoscopic calcaneoplasty is a safe and effective surgery for Insertional Achilles Tendinopathy with Retrocalcaneal Bursitis providing right techniques are used and done by qualified surgeons. The significant advantages are early return to work and sports due to quick postoperative recovery with minimal rehabilitation, small incision, cosmetically acceptable scar and low morbidity.
To Know More
About Orthopedics and
Rheumatology Open Access Journal Please click on:
For more Open Access
Journals in Juniper Publishers please click on:
For more about Juniper Publishers Please click on:



Comments
Post a Comment