Dynamic External Fixation for Unstable Fracture-Dislocations and Pilon Fractures of the Proximal Interphalangeal Joint - Juniper Publishers
Orthopedics and Rheumatology - Juniper Publishers
Abstract
Introduction: Several methods are used in the treatment of intra-articular proximal interphalangeal joint fractures. The purpose of this study was to evaluate the effectiveness of a simple handmade dynamic external fixator for unstable fracture-dislocations and pilon injuries of the PIP joint in an active-duty population and to investigate whether or not these patients had adequate finger movement.
Materials and Methods: Eleven consecutive patients were treated with a simple dynamic external fixator between 2008 and 2014. The analysis of the results was based on the clinical, radiological, and subjective criteria judging Range of Motion of the metacarpophalangeal, proximal interphalangeal, and distal interphalangeal joints, total active motion of the injured finger, and deformity.
Results: The cases included 3 females and 8 males with a mean age of 34 years (range of 19-54 years). The mean follow-up period was 7 months (range, 3–16). Seven patients (77%) attained excellent, 3 (33%) attained good, and 1 (9%) attained fair to poor results. All patients returned to their prior level of activity and duties.
Conclusion: Dynamic external fixation is recommended as the preferred method for dealing with fracture dislocations of the PIP joint because it avoids the soft tissue trauma associated with open surgical techniques. Fixation using this handmade dynamic external fixator for the treatment of the proximal interphalangeal fractures is safe, inexpensive and easy to apply.
Keywords: Dynamic External Fixator; Fracture Dislocation; Proximal Interphalangeal joint; Unstable Fracture-Dislocation; Pilon Fracture; Early Mobilization
Abbreviations: PIPJ: Proximal Interphalangeal Joint; ROM: Range of Motion; DIP: Distal Interphalangeal; TAM: Total Active Motion
Introduction
Injuries to the proximal interphalangeal joint (PIPJ) of the fingers are common. They occur most often following an axial impact on an extended finger. Fractures of the proximal interphalangeal joint include a wide spectrum of injuries, from stable avulsion fractures to complex fracture-dislocations. Stability of the joint is paramount in determining the appropriate treatment, which should aim to facilitate early mobilization and restoration of function.
The purpose of this clinical investigation was to retrospectively review use of simple and handmade dynamic external fixation for unstable fracture-dislocations and pilon injuries of the PIP joint in an active-duty population.
Materials and Methods
A retrospective study was conducted in patients treated with a previously described simple dynamic fixator with no rubber bands(1,2) applied to 11 patients who sustained unstable fracture dislocations or pilon fractures of the PIP joint between 2008 and 2014.
Fracture-dislocation of the PIP was defined as a fracture of the middle phalangeal lip (volar or dorsal) associated with dislocation. An unstable fracture-dislocation was defined as having at least 30% of the articular surface involved, in conjunction with the inability to maintain a concentric reduction of the PIP joint.
The pilon injury type was defined as a fracture in which both the volar and dorsal lips are involved in the fracture. Pilon injuries of the PIP joint are almost always unstable (>1 mm of articular step-off and grossly unstable through full active range of motion). No displaced pilon injuries can be stable; but, this type of injury is rare.
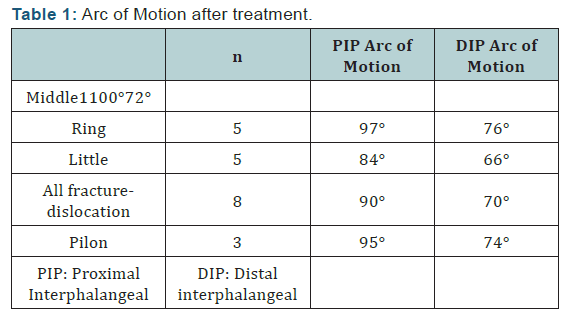
Patients were excluded from the study if they had open injuries or injuries to multiple digits, had sustained a prior injury to the same digit or if they had less than 6 months of follow-up. The injuries occurred in 1 long, 5 ring, and 5 small fingers (Table 1).
All procedures were successfully completed under digital anesthesia without use of sedation, and all patients in our cohort were able to flex and extend at the PIP joint intraoperatively.
Operative Technique
After a closed reduction of the PIP joint fracture-dislocation performed under 31 digital anesthesia and fluoroscopic guidance, a simple frame described by Gaul and Rosenberg [1] and modified by Badia et al. [2] is assembled from two 1.4-mm (0.045-inch) K-wires.
Placement of the K wires is the most critical step. The first K-wire (K1) is placed transversely through the center of the head of the proximal phalanx and the second K-wire (K2) is driven through the head of the middle phalanx (Figure 1a).
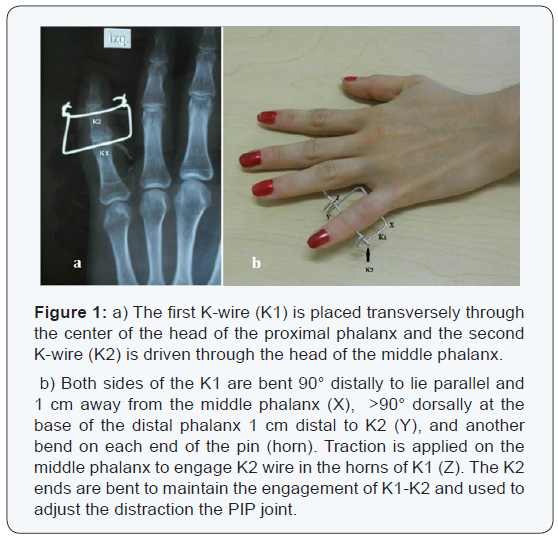
Both sides of the K1 are left long enough so the ends can be bent 90° distally to lie parallel and 1 cm away from the middle phalanx (X) (Figure 1b). Two more bends are applied to the proximal phalanx wire (K1): a dorsal bend (90°) at the base of the distal phalanx approximately 1 cm distal to K2 (Y) (Figure 1b) and another bend on each end of the pin (horn). Traction is applied on the middle phalanx to engage K2 wire in the horns of K1 (Z) of the proximal phalanx (K1) wire, achieving the desired skeletal traction. The K2 ends are bent to maintain the engagement of K1-K2 and used to adjust the distraction the PIP joint (Figure 1b).
Intraoperative x-rays are obtained to confirm that the articular surface of the base of the middle phalanx is not in contact with the condyles of the proximal phalanx. This system provides active longitudinal traction while preserving the joint space and allowing PIP joint motion. The finger is placed in a soft minimally bulky dressing, incorporating the external fixator.
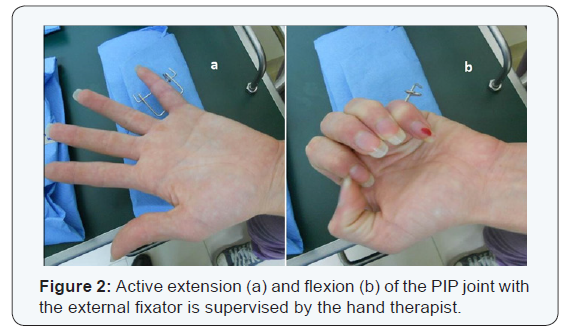
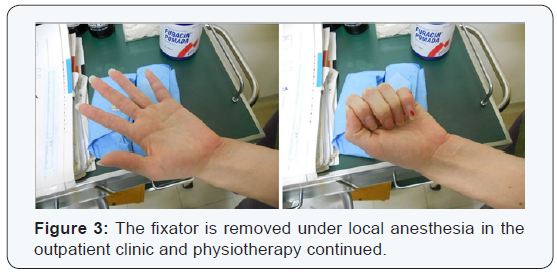
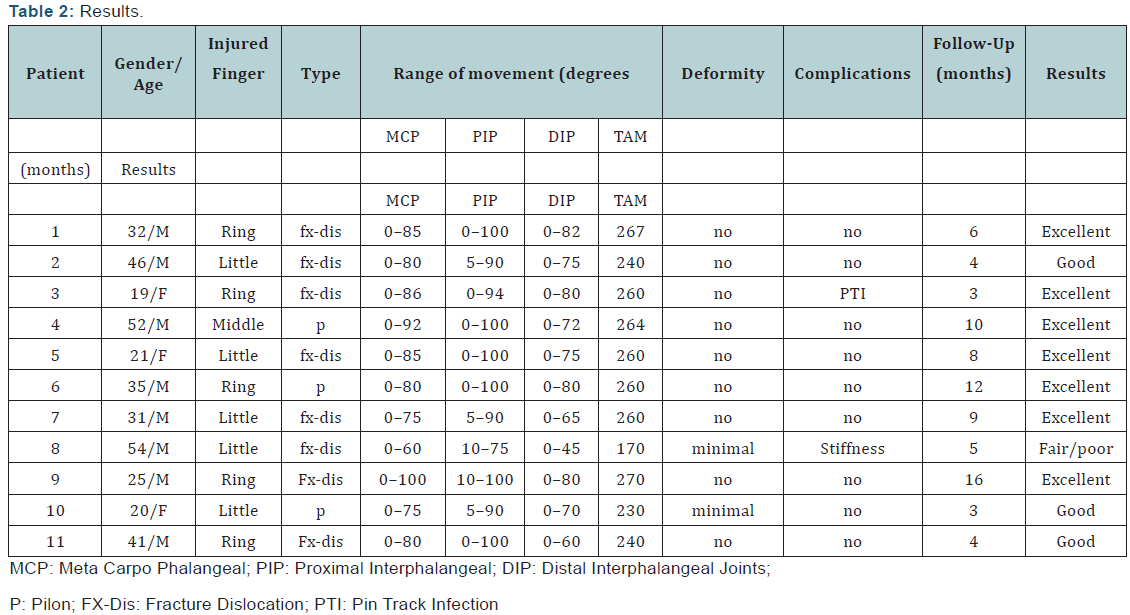
The dressings are removed the next day and immediate active flexion extension of the PIP joint is supervised by the hand therapist (Figure 2) (Supplemental Video 1). Cleansing of the pin sites is performed twice a day with a mixture of iodine and saline. After 4 weeks, the fixator is removed under local anesthesia in the outpatient clinic and physiotherapy continued (Figure 3) (Supplemental Video 2). Radiographic and clinical assessments are obtained at final follow-up evaluation (Table 2).
Functional assessment
The analysis of the results was based on the clinical, radiological, and subjective criteria described in (Table 2), judging Range of Motion (ROM) of the MCP, PIP, and distal interphalangeal (DIP) joints, Total Active Motion (TAM) of the injured finger, and deformity. Each fracture was evaluated and classified according to Rajesh et al. [3] in one of four categories: excellent (pain-free union, no angular/rotational deformity, PIP movement of >100°, total active ROM of >250°); good (occasional pain, minimal angular/rotational deformity, PIP movement of >80°, total active ROM of >180°); and fair to poor (pain, angular/ rotational deformity, PIP movement of ≤80°, total active ROM of ≤180°). Deformity was described as minimal if it was apparent to the physician but was not a functional or cosmetic problem for the patient. Otherwise, results were placed in the fair to poor category.
A Student’s t-test was performed to determine whether the type of fracture (fracture-dislocation vs pilon), or the digit involved (index, long, ring or small finger) had an impact on the final ROM at the PIP and DIP joints.
Results
The cases included 3 females and 8 males with a mean age of 34 years (range of 19-54 years). The mean follow-up period was 7 months (range, 3–16).
At final evaluation no instability was observed in any of the PIP joints. Proper reduction and congruency of the joint was noted on final anteroposterior and lateral radiographs. The average range of motion of the PIP joint at final follow-up evaluation was 3° to 94° (range, 0° to 100°). The final distal interphalangeal range of motion was on average 0° to 71° (range, 0° to 82°).
Seven patients (77%) attained excellent, 3 (33%) attained good, and 1 (9%) attained fair to poor results (Table 2). All patients returned to their prior level of activity and duties.
When comparing the relative effect of digit involved (p=0.02), and fracture-dislocations versus pilon injuries (p=0.006), there were statistically significant differences in PIP joint and DIP joint range of motion.
Those patients who achieved the greatest degree of PIP joint flexion displayed frame translation in conjunction with radiographic evidence of osteolysis in the head of the proximal phalanx. These areas of lysis resolved after removal of the fixator without the need for further intervention.
One patient developed pin tract infection that resolved with oral antibiotics and required premature removal of the fixator (3 weeks).No patient had subsequent surgery.
Discussion
The proximal interphalangeal joint (PIPJ) is the most commonly injured joint in the hand. Although most of these injuries are simple ligamentous sprains, more severe fracture dislocations can occur. Of these, dorsal fracture dislocations are the most common.
The PIP joint is prone to stiffness following even minor sprains; therefore, early diagnosis and treatment of severe fracture-dislocations is essential to achieve optimal function.
Fracture-dislocations of the PIP joint are caused by two basic mechanisms: avulsion or impaction shear. The direction of the middle phalanx versus proximal phalanx is used to categorize the injury as a dorsal fracture-dislocation (i.e., dorsal dislocation with fracture of the middle phalangeal volar lip) or a volar fracture-dislocation (i.e., volar dislocation with fracture of the dorsal lip of the middle phalanx). The third category is a pilon injury in which both the volar and dorsal lips are involved in the fracture [4].
The main concern of management is the stability of the joint. It is determined by the size of the articular fragment of the base of the middle phalanx involved and the degree of impaction of the articular surface.
Unstable fracture-dislocations (at least 30% of the articular surface involved and inability to maintain a concentric reduction of joint) require surgical intervention.
Pilon injuries of the PIP joint are almost always unstable and require surgical intervention. No displaced pilon injuries can be stable and can be managed nonsurgical; but, this type of injury is rare.
When a finger has a painful, unstable PIP joint with a limited arc of motion, overall hand function is greatly impaired. The objectives of treatment of fracture-dislocation of the PIP joint are to reduce the fracture dislocation, allowing early range of motion without compromising stability, prevent posttraumatic arthritis by restoring a congruent joint surface, and optimize functional outcome by maintaining stable range of motion. An aligned and reduced joint is necessary for acceptable clinical outcome [5, 6].
Management of comminuted intrarticular fractures of the base of the middle phalanx poses a therapeutic dilemma. Ideally, anatomic restorations of the joint and early motion are mandatory to minimize posttraumatic arthritis and stiffness. In reality, however, this goal may be impossible because of excessive intraarticular and subchondral comminution.
With regard to the articular surface, quality of reduction has not been shown to correlate with clinically relevant posttraumatic arthrosis in the PIP joint. Several investigators have shown that a small intraarticular step-off can be well tolerated [5].
Several treatment techniques have been described to treat proximal interphalangeal fracture dislocations and pilon fractures of the middle phalanx, including extension block splinting [7,8] or pinning [9], open reduction and internal fixation [10], hemi-hamate arthroplasty [11], volar plate arthroplasty [12,13], skeletal traction [14] force couple splinting [15] and external fixation [1,2,16-18]
The first reference to external fixation for the treatment of PIP fracture-dislocations was in 1946 when Robertson et al. [19] described a triplane external fixation device [19]. Later in 1986, Schenk et al. [20] again proposed the dynamic external fixation method for the treatment of PIP fractures [20].
Many different dynamic external fixators have been described and some of them provide only a traction force, whereas others provide traction as well as a translational force to keep the joint reduced. The ideal dynamic external fixator should be equally effective at maintaining joint reduction as allowing range of motion. It should be inexpensive and easy to apply. We have obtained satisfactory results just by applying the dynamic fixator described by Gaul and Rosenberg [1] and modified by Badia el al. [2]. Only a minor complication (pin tract infection) was reported using this device (Table 1) that resolved with oral antibiotics and required premature removal of the fixator (3 weeks). No patient had subsequent surgery.
The patients who demonstrated the greatest motion with the fixator in place often demonstrated osteolysis around the proximal phalanx axis pin. This can be attributed to the mechanical effect of motion around the pin and was resolved in every case after removal of the fixator. Although differences were noted in final motion based on the finger involved or type of injury (better results middle/ring vs. little finger, and pilon vs. fracture-dislocation type) this study has some weaknesses including small patient cohort and the short length of follow-up. Some loss of motion is expected in nearly all cases of PIPJ fracture-dislocations, regardless of treatment. Nevertheless, a functional, pain-free PIP joint is a reasonable treatment goal in patients with acute injuries.
Conclusion
Dynamic external fixation is recommended as the preferred method for dealing with fracture dislocations of the PIP joint because it avoids the soft tissue trauma associated with open surgical techniques. Fixation using this handmade dynamic external fixator for the treatment of the proximal interphalangeal fractures is safe, inexpensive and easy to apply.
To Know More About Orthopedics and Rheumatology Open Access Journal Please
click on:
https://juniperpublishers.com/oroaj/index.php
For more Open Access Journals in Juniper Publishers please click on:
https://juniperpublishers.com/index.php
For more about Juniper Publishers Please click
on:
https://juniperpublishers0.wixsite.com/juniperpublishers



Comments
Post a Comment