Adjacent Segment Disease after Anterior Cervical Inter body Fusion using Conventional Plate versus Zero-Profile Implant - A Preliminary Report
Orthopedics and Rheumatology - Juniper Publishers
Abstract
Background: Anterior cervical discectomy and interbody fusion is a common surgical method used for treatment of single or 2 level cervical lesion. Recently, zero-profile implant, which lessened irritation of adjacent structures by preventing the contact with them, was design for anterior cervical fusion, and was assumed that it would reduce the occurrence of adjacent segment disease. Thus, authors compared the occurrence of adjacent segment disease after using conventional plate or zero-profile for anterior cervical interbody fusion.
Methods: 48 consecutive cases that underwent single-level anterior cervical discectomy and fusion for lesions of cervical spine that did not respond to nonsurgical treatment and were able to follow up for at least 1 year were included in this study. Clinical and radiologic features of 25 cases (group A) that used conventional plate from April 2007 to January 2011 and 23 cases (group B) that used zero-profile plate from March 2011 to February 2014 were retrospectively compared.
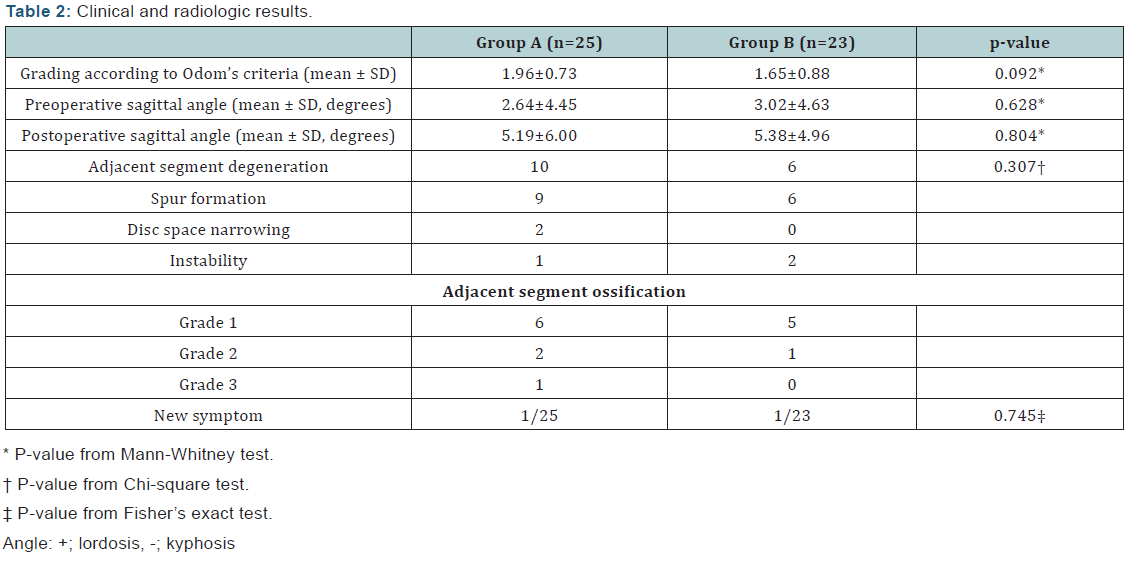
Results: Adjacent segment degeneration was present in 10 cases in group A and 6 cases in group B. The occurrence of the degeneration was statistically insignificant. In aspect of grade of ossification, group A consisted of 6 cases of grade 1, 2 cases of grade 2, and 1 case of grade 3 while group B consisted of 5 cases of grade 1, 1 case of grade 2, and no case of grade 3.
Conclusion: It is considered rather than the insult to adjacent structures by implants, natural degeneration or increased loading to the adjacent segment after interbody fusion are more important factors for occurrence of adjacent segment degeneration.
Keywords: Adjacent segment disease; Anterior cervical inter body fusion; Zero-profile implant
Introduction
Anterior cervical discectomy and fusion is a widely used technique for cervical spine disease and trauma such as herniation of intervertebral disc, cervical spondylotic radiculopathy, cervical fracture, and etc [1]. The technique requires relatively short operation time, has less blood loss and complication, shows immediate symptom relief, and high union rate of over 90% compared to lumbar spine [2]. Though the technique has become popular due to such merits, there are a few possible complications at risk, for example, dysphagia and adjacent segment disease. Adjacent segment disease refers to a radiologic degeneration on the segment adjacent to previous arthrodesis with accompanied symptom due to such degeneration and adjacent segment degeneration refers to only radiologic degeneration. However, the correlation between the degree of degeneration and occurrence of symptom due to degeneration is not well established [3,4]. According to Hilibrand et al, the annual occurrence of adjacent segment disease after anterior cervical discectomy and interbody fusion is about 2.5% [3]. In the other hand, some clinical and mechanical studies reveal that there are no increased motion or pressure of adjacent level after interbody fusion [5,6].
Another study showed that cases with postoperative kyphotic angulation are more likely to have adjacent segment disease [7,8]. As indicative above, numerous studies reported that various factors influence the occurrence of adjacent segment disease and results whether it is brought about due to trauma by surgery or natural history is inconsistent. Based on studies that concluded that adjacent segment degeneration was more frequently occurred and accelerated by insult of tissue due to surgery [9-11], authors investigated the occurrence of adjacent segment disease after anterior cervical discectomy and fusion using zero-profile plate and conventional plate hypothesizing that group using zero-profile plate will show lower occurrence.
Materials and Methods
The study was conducted after the approval of the institutional review board (IRB file no. 2015-08-015). All patients signed consent that they will be enrolled in clinical study. Medical records and radiologic evaluation of 48 consecutive cases that underwent a single level anterior cervical discectomy and fusion due to degenerative change from April 2007 to February 2014 were retrospectively analyzed. All cases had been followed up for at least 12 months clinically and radiologically. Surgery was performed for cases refractory to adequate nonsurgical treatment of at least 6 weeks with a diagnosis of single level cervical radiculopathy or myeloradiculopathy with subtle myelopathy symptoms such as mild numbness on the hand. Patients’ symptoms were well correlated with the conventional radiograph and magnetic resonance images with evident stenosis (Figure 1). The senior author (JS Ahn) performed every surgery and Smith-Robinson technique was used for surgical approach for all patients.
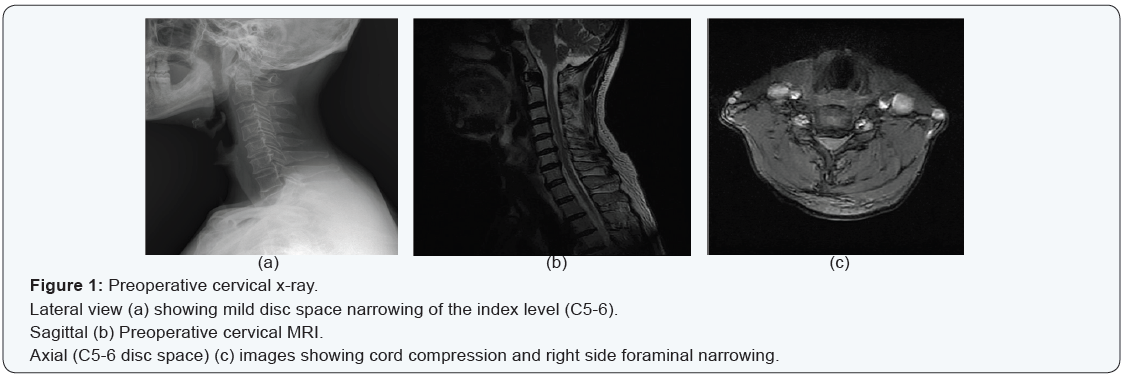
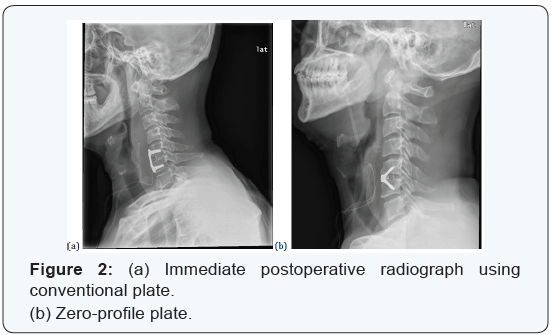
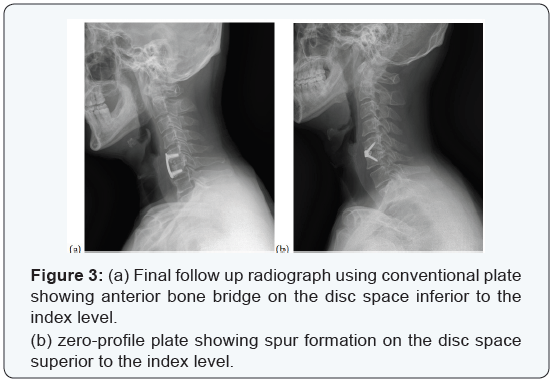
Before the introduction of zero-profile plate on February 2011, a conventional plate (Vectra-T plate, Synthes, Switzerland) was used and ever since, zero-profile plate (Zero-P plate, Synthes, Switzerland) was used for degeneration cases (Figure 2). For postoperative care, soft cervical collar (Philadelphia brace) was applied for 1 day and then all neck motion was allowed without brace. Conventional radiograph was performed on the final follow up for each case (Figure 3). To eliminate the difference of loading due to difference numbers of fused segment, multi segment fusion cases were excluded from the study. In addition, since compromised soft tissues such as anterior longitudinal ligament and bony structures could accelerate degeneration of the adjacent segment, trauma or tumor cases were also excluded [11,12]. Also, cases without radiological follow up at least 12 months after surgery were not included.
Clinical factors such as sex, age, alcohol, smoking, and index level of every patient were checked. The preoperative and postoperative curvature of the index level was measured using simple radiograph. Diagnosis of adjacent segment degeneration and classification of ossification was made according to Katsuura et al. and Nassr et al. [8,9]. Patient was diagnosed as adjacent segment degeneration if at least 1 of the following findings was present:
- Evident intervertebral disc space narrowing
- Newly developed instability on flexion-extension radiographs
- Vertebral anterior or posterior spur formation. Cases were also were classified by the degree of ossification as following:
- Grade 0: no ossification
- Grade 1: extending across less than 50% of adjacent disc space
- Grade 2: extending across more than 50% of adjacent disc space
- Grade 3: complete bridging of adjacent disc space [13].
For evaluate the clinical judgment after surgery, Odom’s criteria along with symptom and sign of each patient were investigated. Odom’s criteria are as follows:
- Excellent: all preoperative symptoms relieved; abnormal findings improved
- Good: minimal persistence of preoperative symptoms; abnormal findings unchanged or improved
- Fair: definite relief of some preoperative symptoms; other symptoms unchanged or slightly improved
- Poor: symptoms and signs unchanged or exacerbated.
- 1 for Excellent,
- 2 for Good,
- 3 for Fair, and
- 4 for Poor
As a result, group A showed 1.96±0.73 points while group B showed 1.65±0.88 points which showed no significant difference between 2 groups (p=0.092). Authors emphasized to keep
For the comparison of diverse clinical factors between two groups, the Mann-Whitney U and chi-squared tests were used. Various pre and postoperative findings were analyzed using the Mann-Whitney U-test, Chi-square test, and Fisher’s exact test. All statistical analysis was performed using the SPSS analytical software version 18.0 (SPSS Inc., Chicago, Ill., USA). In all analyses differences were considered significant at a level of p < 0.05.
Results
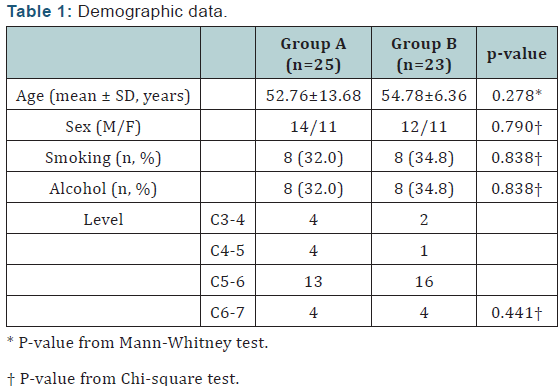
Total of 48 cases were included in the study. 25 cases used conventional plate with cage insertion (group A) and 23 cases used zero-profile plate (group B) for cervical interbody fusion. The demographic data of both groups are descripted on (Table 1). All factors mentioned above showed no statistically significant difference between the 2 groups. Cases’ clinical improvements were graded according to Odom’s criteria:
lordosis of the index level, and as a result, postoperatively, sagittal angle was maintained as a lordotic curve (group A: 5.19±6.00, group B: 5.38±4.96) (+; lordosis, -; kyphosis). Adjacent segment degeneration was present in 10 cases in group A and 6 cases in group B. Specifically, spur formation, disc space narrowing, and instability was found in 9 cases, 2 cases, and 1 case in group A and 6 cases, 0 case, and 2 cases in group B.
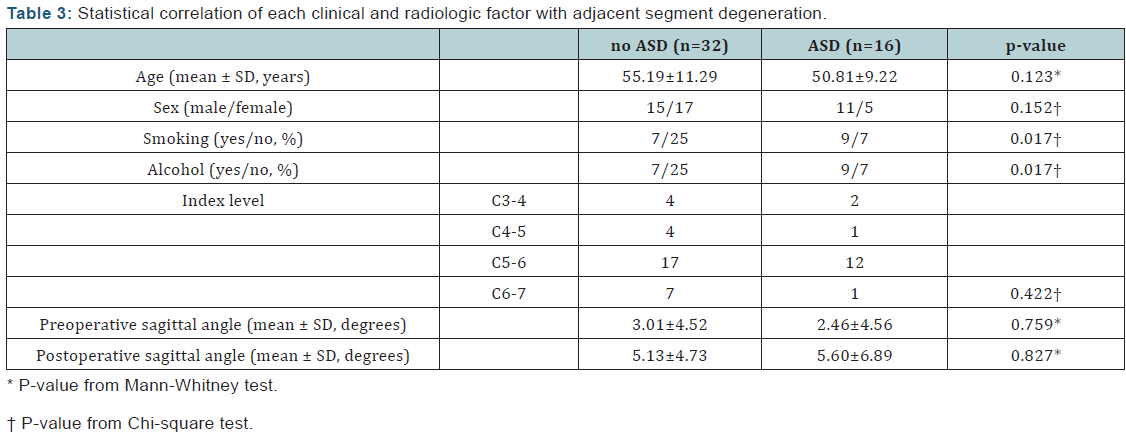
The occurrence of the degeneration was statistically insignificant. (p=0.307) In aspect of grade of ossification, group A consisted of 6 cases of grade 1, 2 cases of grade 2, and 1 case of grade 3 while group B consisted of 5 cases of grade 1, 1 case of grade 2, and no case of grade 3. There were 1 cases of each group that had new radiculopathic symptom (tingling sensation) apart from preoperative symptoms, however, both cases were able to be managed non-surgically (Tables 2 & 3). Each clinical and radiological factor (age, sex, smoking, alcohol drinking, index level, and preoperative and postoperative sagittal angle of the index level) were statistically analyzed for influence to the adjacent segment degeneration. As a result, cases that have smoked and regular alcohol drinker showed a statistically significantly higher occurrence rate of adjacent segment degeneration.
Discussion
Anterior cervical discectomy and fusion is a common procedure for single or two level cervical spondylotic changes or disc disease. Rarely, however, complications of the technique such as postoperative dysphagia, hematoma, recurrent laryngeal nerve, and adjacent segment disease could occur. Specifically, 58.4% of the patients that underwent anterior cervical discectomy and fusion suffered from symptoms related to swallowing difficulty immediately after surgery [2] and among them, 6.6% had the symptom continued until 2 years follow up, [14,15] and adjacent segment disease is reported that the annual occurrence is about 3% [6]. It is assumed that anterior cervical plating bring about dysphagia and adjacent segment disease [16].
However, even with such evidence, most of the anterior cervical discectomy cases are augmented with plating rather than using cage alone since plate augmentation shows higher union rate and preservation of intervertebral disc height [6,17,18]. Thus, to minimize complications while maintain firm fixation with plate, recently a zero-profile plate has been developed and promising results, especially in aspect of dysphagia, are being reported [19-22]. Though the causes of adjacent segment disease is multivariate, however, the issue is that whether it is a result of natural course of degeneration or due to insult after interbody fusion of the cervical spine. Some reports are conflicting with the theory of accelerated adjacent segment degeneration after fusion surgery.
Biomechanical studies by Reitman et al. [5] reported no increased motion of cephalad segment after anterior cervical interbody fusion, and Fuller et al. [23] found that sagittal rotation of the immediately adjacent segment of arthrodesis was not statistically significantly increased. However, there are other studies show contrary results with accelerated degeneration and motion of the adjacent segment after fusion, for example, Eck et al. [24] reported significantly higher intervertebral pressure and motion of the segments adjacent to arthrodesis. Since Park et al. [10] reported that adjacent segment degeneration is prone to occur when the distance of plate end and adjacent disc is less than 5mm and Mahrling [25] reported accelerated degenerative change after wider resection of anterior longitudinal ligament, zero-profile plate was considered to minimize such problems which in order will decrease the occurrence of adjacent segment disease.
However, against to our expectation, according to the result of our study, the difference of occurrence rate between cases using conventional plate and zero-profile plate was statistically insignificant. In view of such result, it is considered that rather than insult to the adjacent segment caused by plating, increased loading to the adjacent segment due to interbody fusion is the major factor for degeneration. In addition, since there are some reports of accelerated degeneration after postoperative kyphotic sagittal alignment [8,26], postoperative sagittal balance should be carefully considered.
There are some limitations of this study, which are small numbers of cases and the results are obtained after a shortterm follow up. Since there is chance of development of adjacent segment problems in longer follow up, which is necessary to make a final conclusion of our study? In addition, as Cherubino et al. [27] described, the degree of degeneration and clinical symptom showed no correlation thus, factors influencing clinical symptoms of adjacent segment was not established. Further evaluation to investigate the factors that cause symptoms due to adjacent segment degeneration is necessary. However, the strength of our study is that, to the best of our knowledge, this is the first study comparing the zero-profile plate with conventional plate in aspect of adjacent segment disease.
Contrary to our expectation, surgery using both implants showed similar results in aspect of adjacent segment degeneration. It is considered rather than the insult to adjacent structures by implants, other factors such as natural degeneration or increased loading to the adjacent segment after interbody fusion might be more important factors for occurrence of adjacent segment degeneration. In short-term after surgery, adjacent segment disease is not a frequently complication, however, longer term follow up is necessary since degeneration of adjacent segment is accelerated.
To Know More About Orthopedics and Rheumatology Open Access Journal Please click on: https://juniperpublishers.com/oroaj/index.php
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com/index.php
For more about Juniper Publishers Please click on: https://juniperpublishers0.wixsite.com/juniperpublishers



Comments
Post a Comment