Treatment of Intertrochanteric Hip Fractures in Elderly High Risk Patients with External Fixation
Orthopedics and Rheumatology - Juniper Publishers
Abstract
In 6 elderly patients intertrochanteric fractures were treated, using FERN external fixation system. All fractures healed within 4 months. Three patients had a superficial pin tract infection and one deep infection. Shortening of 1cm or more was seen in 2 patients. Varus angulation of 5º or more was seen in 2 patients but this seems to be well tolerated by the elderly. External fixation represents an excellent alternative for the surgical treatment of high-risk, elderly patients.
Introduction
Intertrochanteric fractures are very common among elderly patients. These fractures are cause of significant morbidity and mortality in conservatively treated patients. Because of that the treatment of choice is surgery. The most commonly used surgical method is internal fixation which is associated with intraoperative blood loos and prolonged anesthesia. The elderly patients are high risk patients for surgery and conservative treatment is a bad alternative as it is associated with a high mortality rate. The aim of this retrospective study was to evaluate the results of the external fixation for the treatment of intertrochanteric hip fractures in a group of high surgical risk elderly patients.
Patients and Methods.
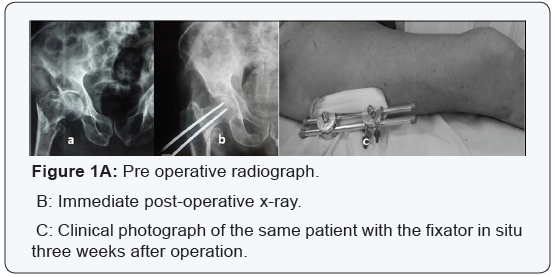
Between 2012 and 2015, 6 elderly high-risk patients classified according to the American Society of Anesthesiologists (ASA) scale (Table 1) sustaining intertrochanteric fractures were treated using the FERN external fixation frame [1]. The fractures were classified according to the modified Evans classification [2] (3 of the fractures were unstable and 5 were stable). Four of these 6 patients were ASA grade III, and 2 were grade IV.
Operative technique
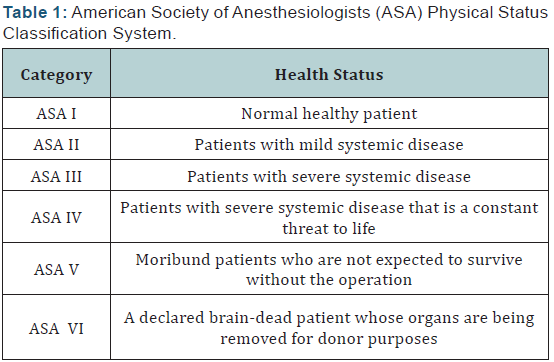
The operations were performed under local anaesthesia with sedation in 2 patients, in rest of the patients short spinal or epidural anaesthesia was used. After placing the patient on the fracture table a closed reduction of the fracture was performed under image intensification. Fracture was fixed with two 5 mm
diameter and 20-25 cm long thread pin with sharp tip passed from lateral aspect greater trochanter along the neck engaging the subchondral bone of head. Two or three more thread pins were passed in the proximal femur. All the pins were connected with an external rod (Figure 1). Stability of fracture fixation was checked under image intensifier using varus- vulgus stress. The patients were given prophylactic antibiotics, lowmolecular heparin, and analgesics. The patients were made to sit up immediately postoperatively and limited non-weight bearing ambulation for up to 6 weeks after which gradual increase from toe-touch to full weight bearing was instituted. Patient’s family was also educated for the physiotherapy (hip, knee and chest) and pin tract care. External fixator was removed without anaesthesia in outpatient clinic after radiological evidence of fracture union.
Results
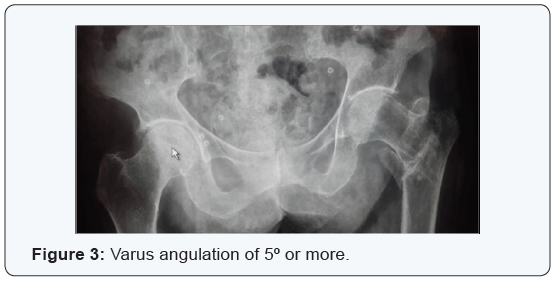
No patient needed blood transfusion intra operatively or post operatively. The average follow up was 5.2 months ranging from 3 months to 18 months. The average operative time was 38 ± 2 minutes. The average duration of hospitalization was 5 days (range: 3 to 8). All fractures have radiological union at 4 months (Figure 2). One patient had died 9 months post-operatively due to causes unrelated to external fixator application. Pin tract infection was the most common complication, 3 patients were affected by superficial pin tract infection which resolved with cleaning and dressing with chlorhexidine, without administration of antibiotics. Shortening of 1cm or more was seen in 2 patients. Varus angulation of 5º or more was seen in 2 patients (Figure 3).

They followed their patients for an average of 26 months (12 -51 months). There were 2 non-unions; one patient was treated with cast and the other with a plate. There were 13 patients with open fractures. It is not clear how patients were allocated. However, the methods laid the foundation for the management of segmental tibial fractures. The implants have improved over the years but the principles of treatment have not changed dramatically over these years. In 1969, Zucman and Maurer [6] introduced the technique of unreamed tibial nailing in the management of both closed and open segmental fractures. There was no grading of open fractures as we know it today. They found that 19/36 (79%) of open fractures achieved union without complications. There were two cases of non-union of closed fractures. Deep sepsis developed in four cases (12%); two of these united without any surgical intervention. Tibial nailing was to be the major technique in the management of these fractures as will be evident in subsequent cases.
Functional outcome of segmental tibial fractures was not documented in the majority of previous reports. Oivind & Olav [7] reviewed 54 patients with the aim of documenting functional outcome. They found that 53.7% of their patients had full recovery and the rest had some form of functional impairment. Their assessment was to have great impact to subsequent authors: it was clear that closed segmental fractures should be viewed differently from open ones. It was Melis et al. [8] who, in their reviews of 38 patients separated the treatment of open and closed segmental tibial fractures. They used reamed K-nail- Hertzog nail. Open fractures were treated with antibiotics for 20 days plus continuous irrigation and suctioning for at least 10 days. Soft tissue coverage was done after 10 days. They clearly documented all complications which occurred that included skin breakdown, melanin and sepsis.
They noted that skin breakdown did occur in closed fractures as well. Woll & Duwelius [4] used Ender nails in both closed and open fractures. All fractures united. The few complications they encountered included superficial sepsis, DIC, shortening and melanin. Complications associated with this kind fracture were mal-union and shortening. But in our patient it was not the case. At follow up patient recovered well with no residual co morbidity. Giannoudis et al. [1] findings send a very important message that “66.6% of segmental tibial fractures require more than one surgical intervention”. It is therefore extremely vital to plan ahead so that should subsequent surgical interventions become necessary, the surgeon is well prepared for it. This
planning ahead implies re-aligning the medullary cavity from the start.
Discussion
Hip fracture is a leading cause of death and disability among the elderly [3]. Delay in operation is associated with an increased risk of morbidity and mortality [4]. The mortality rate associated with these fractures is 10-30% in first year after trauma [5]. An increased mortality rate after fracture of the hip is associated among other factors with advanced age, untreated or poorly controlled systemic disease, and control of medical co morbidities [6]. Although internal fixation is the gold standard for fixation of these fractures, it may not always be possible to undertake this procedure elderly high risk patients In such circumstances, external fixation is a good alternative for fracture stabilization allowing for a quick, cheap and effective stabilization that can be undertaken even under local anesthesia [7].
External fixation was introduced for the management of trochanteric fractures at about the same time as the first sliding internal fixation devices [8,9] but its use has decreased considerably in recent years. Studies comparing external fixation to sliding hip screws have reported superior outcomes in favor of external fixation [10-12]. Complications related to external fixator include pin tract infection which can easily be controlled with meticulous local care. In our study superficial pin tract infection was the most common complication (3 patients) which resolved with cleaning and dressing with chlorhexidine, without administration of antibiotics. Varus angulation of 5º or more was seen in 2 patients. Collapse of the fracture into varus is commonly found in in grossly unstable fractures but this seems to be well tolerated by the elderly, possibly because of their low demands in activities of daily living or due to associated co-morbidities restricting excessive ambulation [13].
Conclusion
External fixation provided an excellent alternative for the treatment in elderly high risk patients with intertrochanteric hip fractures for open surgery which offers a low-risk operation with minimal blood loss, fast mobilization, few postoperative complications, and reduced cost because of the short hospitalization.
To Know More About Orthopedics and Rheumatology Open Access Journal Please click on: https://juniperpublishers.com/oroaj/index.php
For more Open Access Journals in Juniper Publishers please click on: https://juniperpublishers.com/index.php
For more about Juniper Publishers Please click on: https://juniperpublishers0.wixsite.com/juniperpublishers



Comments
Post a Comment